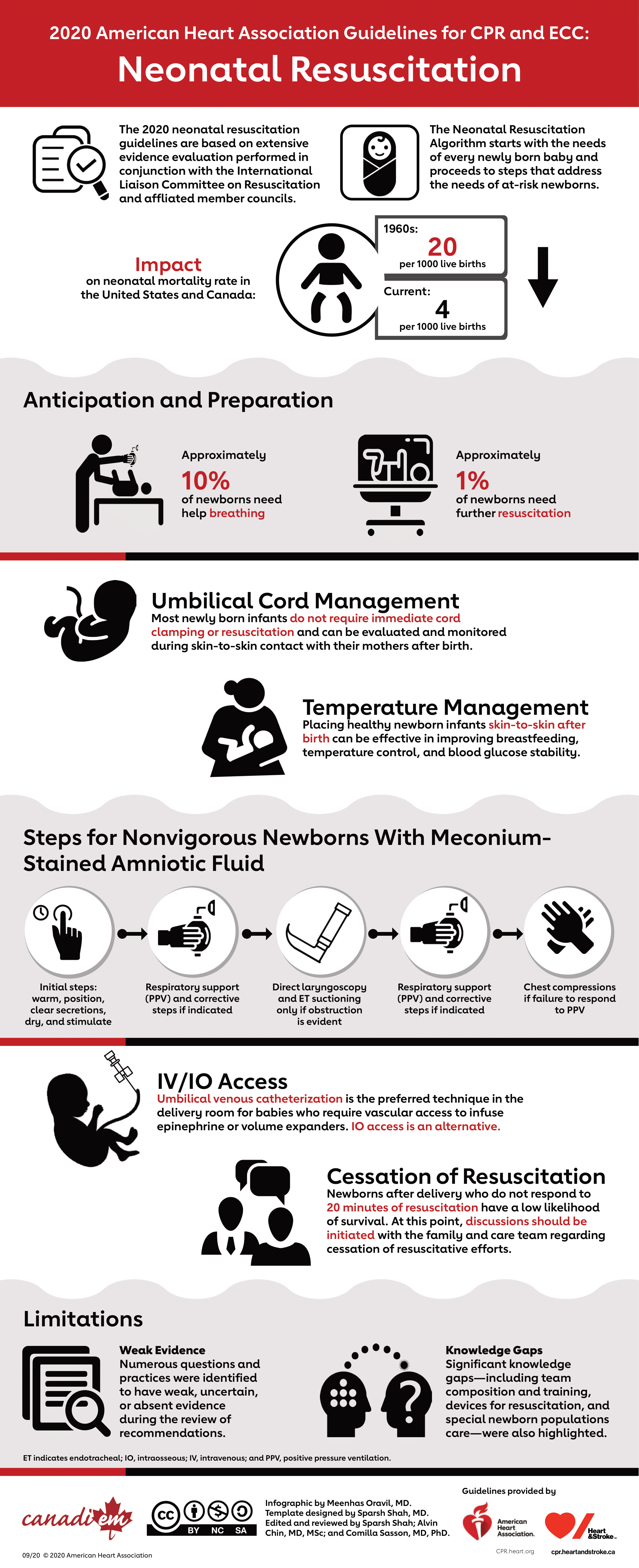
This year, the American Heart Association released the updated 2020 Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care; the first update to the internationally recognized guideline in five years.
The top ten things to know for Neonatal Guidelines are as follows:
1. Anticipation and Preparation: Newborn resuscitation depends heavily on proper planning and readiness of the team. Effective team behaviors, such as anticipation, communication, briefing, equipment checks, and assignment of roles, result in improved team performance and neonatal outcome.
2. Cord management: Most newly born infants do not require immediate cord clamping or resuscitation and can be evaluated and monitored during skin-to-skin contact with their mothers after birth.
3. Positive-pressure ventilation and Oxygen therapy: PPV remains the primary method for providing support for newborns who are apneic, bradycardic, or demonstrate inadequate respiratory effort. Pulse oximetry is used to guide oxygen therapy and meet oxygen saturation goals. A rise in heart rate is the most important indicator of effective ventilation and response to resuscitative interventions.
4. Chest compressions: If the heart rate remains less than 60/min despite 30 seconds of adequate PPV, chest compressions should be provided. The suggested ratio is 3 chest compressions synchronized to 1 inflation (with 30 inflations per minute and 90 compressions per minute) using the 2 thumb–encircling hands technique for chest compressions.
5. Temperature Management: Placing healthy newborn infants skin-to-skin after birth can be effective in improving breastfeeding, temperature control, and blood glucose stability.
6. Vascular access: When vascular access is required in the newly born, the umbilical venous route is preferred. When intravenous access is not feasible, the intraosseous route may be considered.
7. Medications: If the response to chest compressions is poor, it may be reasonable to provide epinephrine, preferably via the intravenous route.
8. Volume expansion: Failure to respond to epinephrine in a newborn with history or examination consistent with blood loss may require volume expansion.
9. Withholding and discontinuing resuscitation: If all these steps of resuscitation are effectively completed and there is no heart rate response by 20 minutes, redirection of care should be discussed with the team and family. Appropriate and timely support should be provided to all involved.
10. Knowing the limitations: Teams and individuals who provide neonatal resuscitation are faced with many challenges with respect to the knowledge, skills, and behaviours needed to perform effectively. Neonatal resuscitation teams may therefore benefit from ongoing booster training, briefing, and debriefing.

Further reading:
Heart & Stroke 2020 Guidelines for CPR and Emergency Cardiovascular Care
American Heart Association 2020 Guidelines for CPR and Emergency Cardiovascular Care